Non-surgical Rehabilitation
If at all possible, you must change or stop all activities that cause your symptoms. Take frequent breaks when doing repeated hand and thumb actions. Avoid repetitive hand motions such as heavy grasping, wringing, or turning and twisting movements of the wrist. Keep the wrist in a neutral alignment. In other words, keep it in a straight line with your arm, without bending it forward or backward.
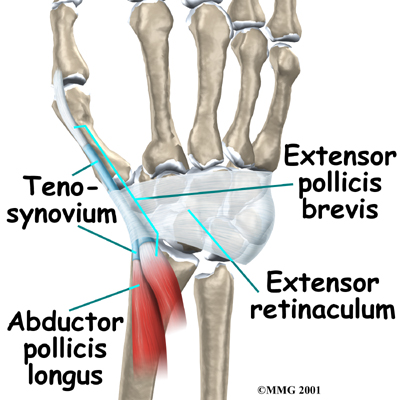
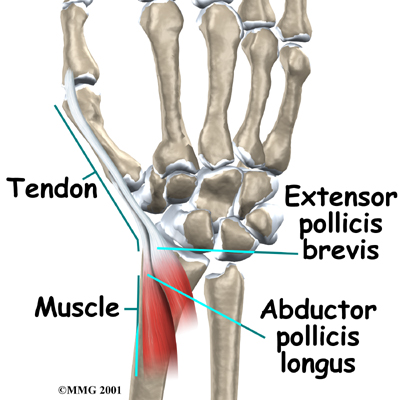
 After your injury is evaluated, our Physical Therapist may want you to wear a special forearm and thumb splint called a . This splint keeps the wrist and lower joints of the thumb from moving. The splint allows the APL and EPB tendons to rest, giving them a chance to begin to heal.
After your injury is evaluated, our Physical Therapist may want you to wear a special forearm and thumb splint called a . This splint keeps the wrist and lower joints of the thumb from moving. The splint allows the APL and EPB tendons to rest, giving them a chance to begin to heal.
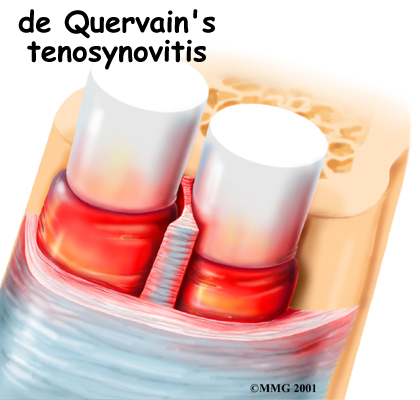
Anti-inflammatory medications may also help control the swelling of the tenosynovium and ease symptoms. These medications include common over-the-counter medications such as ibuprofen and aspirin.
When you begin your STAR Physical Therapy program, the main focus of our Physical Therapy is to reduce or eliminate the cause of irritation of the thumb tendons. Our Physical Therapist may check your workstation and the way you do your work tasks. We may provide suggestions about the use of healthy body alignment and wrist positions, helpful exercises, and tips on how to prevent future problems.
If nonsurgical treatment is successful, you may see improvement in about four to six weeks. You may need to continue wearing your thumb splint to control symptoms. Try to do your activities using healthy body and wrist alignment, and limit activities that require repeated motions of the wrist and thumb.
Post-surgical Rehabilitation
Rehabilitation is more involved after surgery. Full recovery could take several months. Pain and symptoms generally begin to improve after surgery, but you may have tenderness in the area of the incision for several months.
Take time during the day to support your arm with your hand elevated above the level of your heart. You should move your fingers and thumb occasionally during the day. Keep the dressing on your hand until you return to the surgeon. Avoid getting the stitches wet. Your stitches will be removed 10 to 14 days after surgery.
Although the time required for recovery is different for each patient, as a general rule, you will probably need to attend your Physical Therapy sessions for six to eight weeks. Our therapist will have you begin by doing active hand movements and range-of-motion exercises. We may also use ice packs, soft-tissue massage, and hands-on stretching to help with the range of motion.
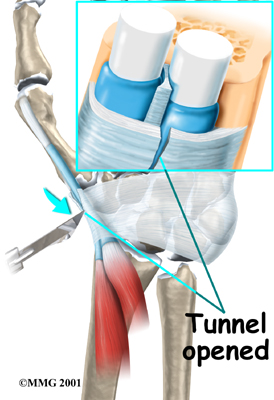
When the stitches are removed, you may start carefully strengthening your hand and thumb by squeezing and stretching putty. Our Physical Therapists also use a series of gentle stretches to encourage the thumb tendons to glide easily within the tunnel.
As you progress, our Physical Therapist will give you exercises to help strengthen and stabilize the muscles and joints in your hand and thumb. We may also use other exercises to improve fine motor control and dexterity. Some of the exercises we’ll recommend are designed to get your hand working in ways that are similar to your work tasks and sport activities.
Our Physical Therapist will help you find ways to do your tasks that don't put too much stress on your thumb and wrist. Before your Physical Therapy sessions end, our Physical Therapist will teach you a number of ways to avoid future problems.
STAR Physical Therapy provides services for Physical Therapy in Fairport and Rochester.
 After your injury is evaluated, our Physical Therapist may want you to wear a special forearm and thumb splint called a
After your injury is evaluated, our Physical Therapist may want you to wear a special forearm and thumb splint called a